Let’s Talk about Endometriosis
Endometriosis is a disease we are finally hearing about more and more often, but it is still not being taken seriously. In the UK, 1 out of 10 women suffers from it. And yet, it takes on average 7.5 years to get a firm diagnosis. 7.5 years! Can you believe that?
What’s endometriosis
Endometriosis is a condition where endometrial cells that usually constitute the “wallpaper” of your uterus are present somewhere else, e.g. the ovaries or the fallopian tubes or even other places in your body.
Every month the “wallpaper” of your uterus is replaced: that’s when you have your periods. But if you have endometrium in other places, it has nowhere to go and this can cause a lot of pain.
The cause of endometriosis is still unknown. There are several theories, but nothing is known for sure at the moment. If you want to know more, I suggest reading this review paper on the subject.
Symptoms
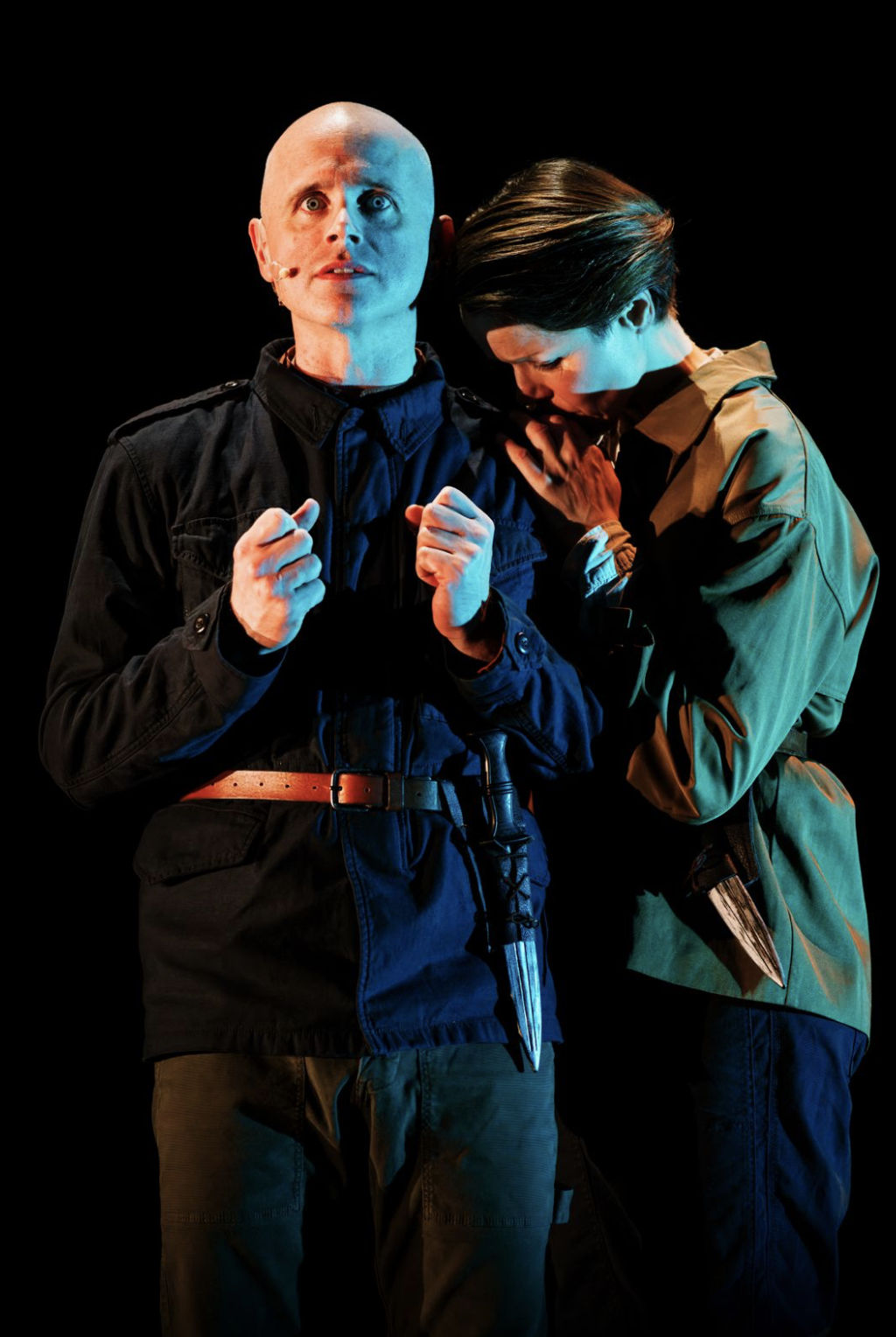
Women can suffer from a variety of symptoms such as chronic pain in the lower abdomen especially during periods, heavy and very painful periods, pain during and/or after sexual intercourse, bowel and/or bladder troubles, infertility problems. Symptoms can be constant or cyclical.
The intensity of these symptoms may differ from one woman to another. Some women are in such pain that it disturbs their entire life either their working life or their social life or their sexual life or all of the above. This can lead to isolation and depression.
Some other women can be asymptomatic, which can make the diagnosis even more difficult (but their life easier).
How to be sure you have endometriosis
That’s when it gets tricky. The problem is that these symptoms may be misleading, as they can be associated with other conditions. And when you describe them to your GP, she or he may not think of endometriosis in the first place
Vaginal examinations, blood and urine tests, and scans can help diagnose endometriosis but without any certainty.
The only way to diagnose endometriosis is by having a laparoscopy, an operation where a surgeon inserts a camera into the pelvis to look for any misplaced endometrial cells. And yet, if you actually have bladder endometriosis, a laparoscopy won’t show it. You would need a cystoscopy instead (a camera inserted in your urethra to see your bladder lining).
Because of all that, having a definite diagnosis can take several years. To accelerate the process, I would suggest daily writing all your symptoms down in a diary. Write when you feel sick, where it hurts, the intensity of the pain etc... Write when you feel good as well.
You know your body better than your GP and writing everything down will help you see patterns. You can then talk to your GP about it and this may accelerate the diagnosis.
Treatments and information
Having the proper treatment is another battle. First, you could be offered some painkillers and pain management options. Finding the medicine that works for you may take some time and this may be frustrating.
You could be offered a hormone treatment such as a contraceptive pill, which will block ovulation and reduce the endometrial symptoms. This is usually offered to women with mild symptoms.
If you have intense symptoms, you could have surgery to remove the misplaced endometrial tissues. Depending on how much the endometrial tissues have spread, you may need multiple surgeries, and these can be hard to cope with.
For more information about endometriosis, visit the endometriosis UK website. The website is full of helpful tips (which helped me write this article). If you need to talk to somebody, they have a free helpline. You’re not alone in this battle.
My personal story
I found out that I had endometriosis 3 years ago when I was in Chile. While I was there, I decided to stop the contraceptive pill that I had been taking for 14 years. And a month later, I was in hell. I had intense pelvic pain, I couldn’t remain standing for too long, going for a walk was a challenge, sleeping was very difficult, focusing at work was almost impossible.
I had no idea what was going on. I went to a first doctor who thought it was cystitis, so I got a urine test and antibiotics. Then another doctor thought it was a fungus infection, so I got a vaginal examination and antifungal meds. I saw a gynaecologist who told me this pain was normal after stopping a contraceptive pill, so I got another vaginal examination and pain killers.
At some point, I had so many pills that didn’t even know what I was taking. And I was still in deep pain. Being in a foreign country all by myself with this going on was really isolating. And this went on for several months.
Then, I started recording everything I was feeling and went to an endometriosis specialist. I got another vaginal examination and a hysteroscopy (a camera inserted in the vagina). He told me that there was a high chance that I had endometriosis, but he couldn’t know for sure.
The story gets a bit political because in Chile, the health system is messed up. I won’t go into the details, but I was so fed up that I decided to try a different contraceptive pill and stop going to doctors. I feel very lucky that the pill worked, and I could have my life back. I know it’s not the case for many women.
If you have symptoms, talk to your GP about endometriosis and make sure you get a laparoscopy. Having a firm diagnosis is often a relief even though it’s not the end of the battle. Seek out help, don’t isolate yourself because of this disease. And remember, you’re not alone in this: 1 out 10 women are in the same situation.
Help us keep the City Girl Network running by supporting us via Patreon for the price of a cheap cup of coffee- just £2 a month. For £3 a month you can also get yourself a Patreon exclusive 10% off any of our ticketed events! You can also support us by following us on Instagram, and by joining our City Girl Network (city-wide) Facebook group.
Elise Van Meerssche